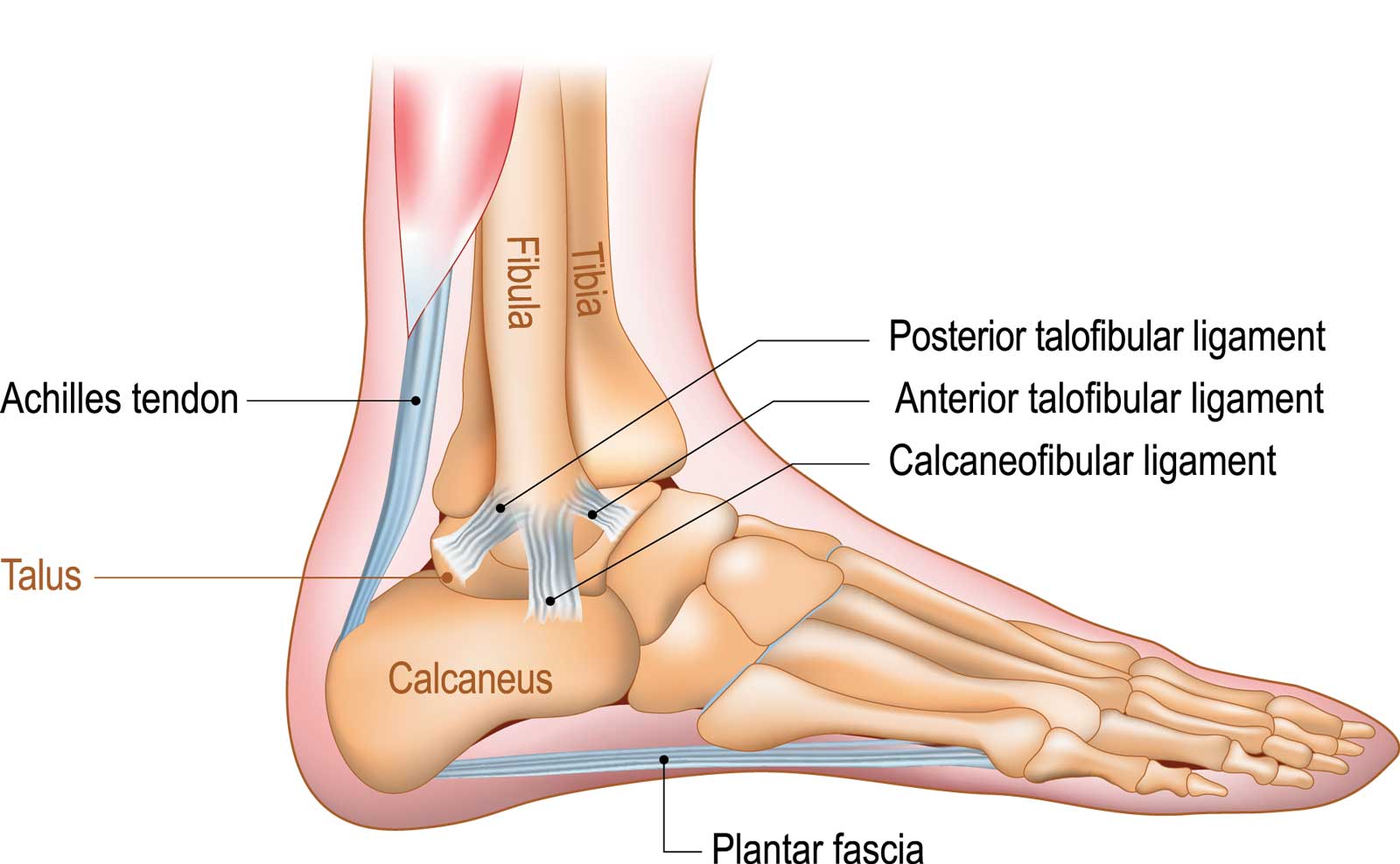
Plantar fasciitis is the most common cause of pain on the bottom of the heel, with approximately two million individuals treated for this condition every year. Plantar fasciitis occurs when the strong band of tissue that supports the arch of your foot becomes irritated and inflamed, resulting in heel pain.
This condition is sometimes called heel spur syndrome when a spur is present. Heel pain may also be due to other causes, such as a stress fracture, tendonitis, arthritis, or nerve irritation. Because there are several potential causes, it is important to have heel pain properly diagnosed. Your foot and ankle specialist is able to distinguish between all the possibilities and determine the underlying source of your heel pain.
Symptoms of Plantar Fasciitis
The symptoms of plantar fasciitis include:
- Pain on the bottom of the heel
- Pain that is usually worse upon arising
- Pain that increases over a period of months
People with plantar fasciitis often describe the pain as worse when they get up in the morning or after they’ve been sitting for long periods of time. After a few minutes of walking, the pain decreases because walking stretches the fascia. For some people the pain subsides but can return after spending long periods of time on their feet.
What Causes Plantar Fasciitis
The most common cause of plantar fasciitis relates to a faulty structure of the foot. People who have problems with their arches, overly flat feet, or high-arched feet are more prone to developing plantar fasciitis.
Wearing non-supportive footwear on hard, flat surfaces puts abnormal strain on the plantar fascia and can lead to plantar fasciitis. This is particularly evident when your job requires long hours on you feet. Obesity may also contribute to plantar fasciitis.
Treatment for Plantar Fasciitis
Conservative Treatment
- Stretching Exercises – Exercises that stretch out the calf muscles will help ease pain and assist with recovery.
- Avoid going barefoot – When you walk without shoes, you put undue stress and strain on your plantar fascia.
- Ice – Putting an ice pack on your heel for 20 minutes several times a day helps reduce inflammation. Place a thin towel between the ice and your heel and do not apply ice directly to the skin.
- Limit Activities – Cut down on extended physical activities, giving your heel a rest.
- Shoe Modifications – Wearing supportive shoes that have good arch support and a slightly raised heel reduces stress on the plantar fascia.
- Medications – Oral nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be recommended to reduce pain and inflammation.
Advanced Conservative Treatment
- Padding and Strapping – Placing pads in the shoe softens the impact of walking. Strapping helps support the foot and reduce strain on the fascia.
- Orthotic Devices – Custom orthotic devices that fit into your shoe help correct the underlying structural abnormalities causing the plantar fasciitis.
- Removable Walking Cast – A removable walking cast may be used to keep your foot immobile for a few weeks, allowing it to rest and heal.
- Night Splint – Wearing a night splint allows you to maintain an extended stretch of the plantar fascia while sleeping. This may help reduce the morning pain experienced by some patients.
- Physical Therapy – Exercises and other physical therapy measures may be used to help provide relief.
Regenerative Treatment
Regenerative medicine offers effective solutions for chronic plantar fasciitis. PRP therapy uses concentrated platelets from your blood to reduce inflammation and promote healing in the plantar fascia. Stem cell therapy, using cells harvested from your own fat, can help repair and strengthen the damaged tissue. These minimally-invasive treatments can provide long-lasting relief when conservative measures aren't enough.
Surgical Treatment
Although most patients with plantar fasciitis respond to non-surgical treatment, a small percentage of patients may require surgery. If, after several months of non-surgical treatment, you continue to have heel pain, surgery will be considered. Your foot and ankle surgeon will discuss the surgical options with you and determine which approach would be most beneficial for you.
No matter what kind of treatment you undergo, the underlying causes that led to plantar fasciitis may remain. You should continue with preventive measures, such as wearing supportive shoes, stretching, and using custom orthotic devices.
