What are Metatarsal Fractures?
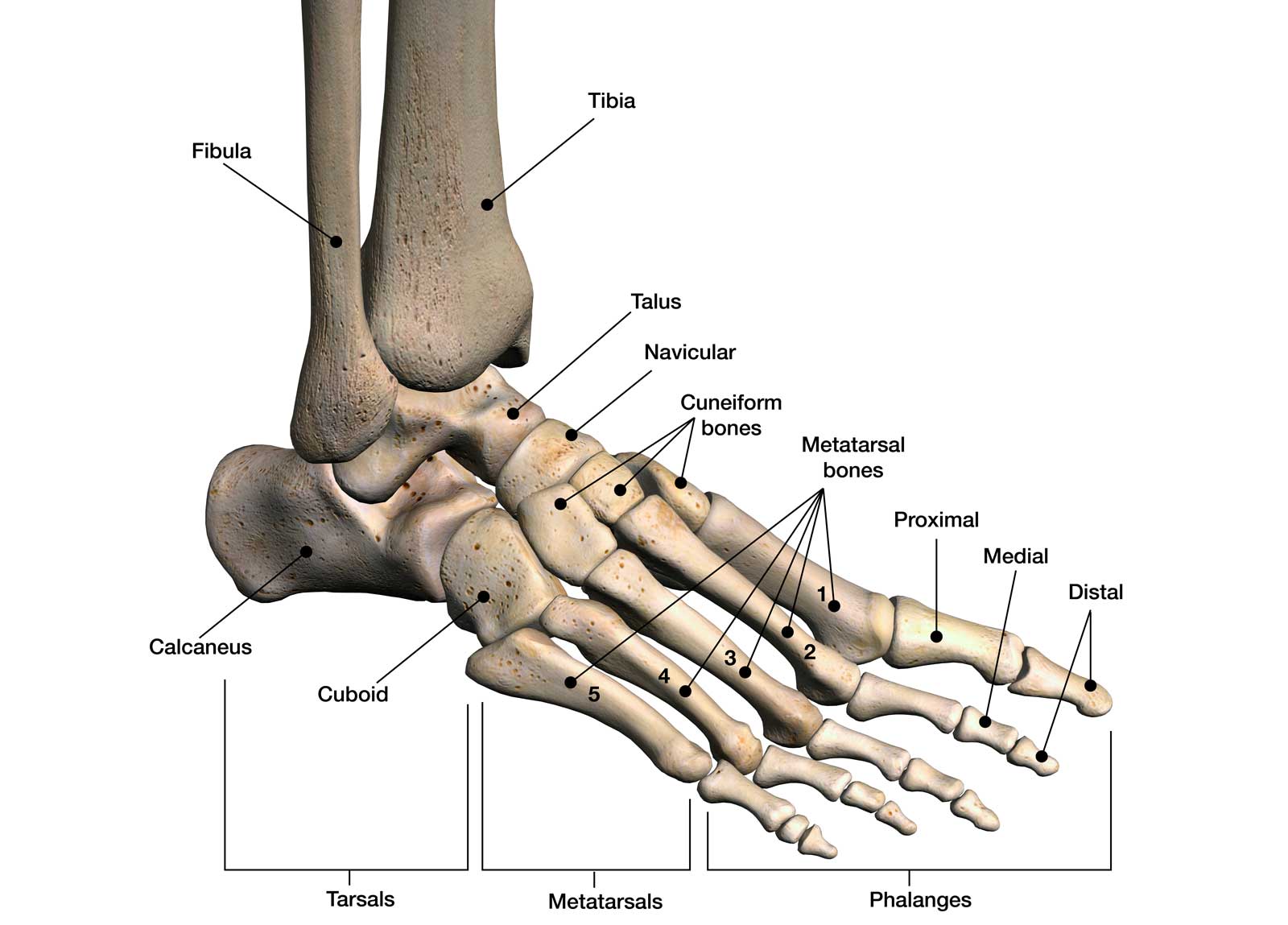
There are five metatarsal bones in each foot. These bones play a crucial role in weight-bearing and movement, making metatarsal fractures a significant injury that can impact mobility and daily activities. Fractures can range from small, hairline cracks to complete breaks, and they can occur in any of the five metatarsal bones.
Types of Metatarsal Fractures
Metatarsal fractures are typically categorized based on their location and the nature of the break. Common types include:
- Shaft fractures occur in the long, middle portion of the metatarsal bone. These can be transverse (straight across the bone), oblique (at an angle), or spiral (winding around the bone).
- Neck fractures happen near the end of the metatarsal bone, close to the toe joint. These are often seen in the fifth metatarsal.
- Base fractures occur at the end of the metatarsal bone closest to the ankle. A particularly common type is the Jones fracture, which affects the fifth metatarsal base and can be challenging to heal due to poor blood supply in this area.
- Stress fractures are tiny, hairline breaks that typically result from repetitive stress or overuse. They're common in athletes and can affect any of the metatarsals.
Metatarsal fractures can occur due to various reasons. Acute fractures often result from direct trauma, such as dropping a heavy object on the foot, or from twisting injuries during sports or falls. Stress fractures, on the other hand, develop over time due to repetitive force or overuse.
Symptoms of a Broken Metatarsal
The symptoms of a metatarsal fracture can vary depending on the type and severity of the break. In cases of acute fractures, patients typically experience sudden, severe pain at the site of the injury. This is often accompanied by swelling, bruising, and difficulty walking or bearing weight on the affected foot. There may also be visible deformity in severe cases.
Stress fractures tend to have more gradual onset of symptoms. Patients might notice pain that worsens with activity and improves with rest. There may be tenderness and swelling over the affected area.
In both types of fractures, pain typically increases when pressure is applied to the injured area or when attempting to push off with the affected foot during walking.
Diagnosis and Treatment
As with any broken bone, imaging studies play a key role in diagnosis. X-rays are usually the first imaging test performed, providing clear views of the bones to identify fractures, their location, and severity. In some cases, especially for suspected stress fractures that may not be visible on regular X-rays, additional imaging such as MRI or bone scans may be necessary. These advanced imaging techniques can detect subtle changes in the bone that indicate a stress fracture or other soft tissue injuries, such as plantar fasciitis, that may be contributing to the pain.
Treatment for metatarsal fractures varies depending on the type, location, and severity of the fracture, as well as the patient's overall health and activity level. The primary goals of treatment are to promote proper bone healing, relieve pain, and restore function to the foot.
For many metatarsal fractures, non-surgical treatment is sufficient. This typically involves a period of immobilization using a cast or walking boot. As healing progresses, a gradual return to weight-bearing activities is allowed under the guidance of the treating physician.
Surgical treatment may be necessary for certain types of metatarsal fractures, particularly those that are displaced (where the bone ends are out of alignment), open fractures (where the bone has broken through the skin), or fractures that fail to heal with conservative treatment. Surgery typically involves realigning the bone fragments and securing them in place with screws, plates, or pins.
Recovery and Rehabilitation
Recovery from a metatarsal fracture can take several weeks to months, depending on the severity of the injury and the treatment method. As healing progresses, rehabilitation plays a crucial role in restoring strength, flexibility, and function to the foot.
Physical therapy often begins with gentle range of motion exercises and gradually progresses to strengthening exercises and activities to improve balance and proprioception. Your physical therapist will also work with you on gait training to ensure proper walking mechanics as you return to full weight-bearing. For athletes or highly active individuals, sport-specific training may be incorporated into the later stages of rehabilitation to facilitate a safe return to previous activity levels.
If you've experienced a foot injury or are dealing with persistent foot pain, don't hesitate to seek expert care. Contact us today to schedule a consultation.
